Menopause can often be very readily dismissed as being simply a hot flash or two. It is so much more, but a severe lack of understanding and awareness can diminish the experience of anyone going through menopause. This can result in questions not being asked, limiting the possibility of making informed choices. When it comes to menopause, there are no awkward or ridiculous questions. Learning about menopause is critical. Always ask.
Dr Caoimhe Hartley founded Menopause Health in 2021 to help women access the best advice and care throughout menopause. Dedicated to women's health, Dr Hartley is conscious of the difficulties women experience in understanding and navigating their menopause journey. Dr Deirdre Lundy from the Bray Women's Health Centre is a specialist in women's health and oversees menopause training for Irish GPs at the Irish College of General Practitioners.
They respond here to some of our concerns about menopause.
I’m 49 but don’t feel menopausal. Does every woman get menopause symptoms?
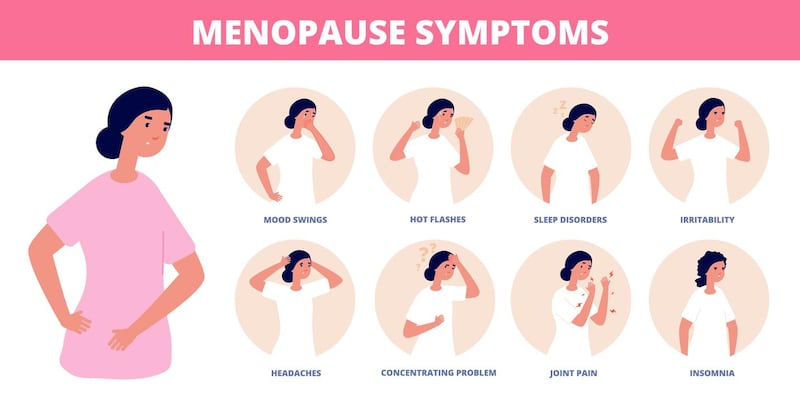
“The majority of women will experience some perimenopausal or menopausal symptoms,” says Dr Hartley. “It can affect their mood, their sleep, or physical symptoms such as hot flashes or night sweats. For some women, it may be vaginal dryness or bladder symptoms. The bone density loss which happens when our oestrogen production falls at menopause is, for the most part, silent.
“However, thankfully, there is a percentage of women who have no symptoms at all. Similarly, not all women have significant bone density loss after menopause. Why some women have symptoms and others don’t may depend on genetic factors. If your periods have stopped for more than one year [and you are over the age of 50], you can be confident that you are menopausal.”
My body aches. Is this a sign of menopause?
“Generalised aches and pains are common in menopause,” advises Dr Hartley. “This may be due to the loss of oestrogen, which has some weak anti-inflammatory properties. Similar symptoms have been shown to occur with aromatase inhibitors which are anti-oestrogen medications, sometimes used in patients who have had breast cancer.
“There can be a knock-on effect of these aches, including poor sleep and a reduced ability to enjoy exercise or be active. Living with aches and pains can also have a negative impact on our mood. You may find that an old injury flares up, or it could be a totally new symptom. Know that you are not alone and that there are options available to help. Joint aches and pains can also be due to other causes such as osteoarthritis, inflammatory arthritis and other conditions. It is always a good idea to discuss this with your GP as you may need further investigation.”
My symptoms are relentless. What can I do?
“Lots,” reassures Dr Hartley. “First step is to reach out for advice and help. Don’t suffer in silence! The management route will depend on what symptoms you are experiencing, what background health risks and values you may have. I usually start by chatting to patients about lifestyle interventions, exercise, CBT [cognitive behavioural therapy], reducing caffeine and alcohol, and a discussion about sleep hygiene, etc.
“There are non-hormonal and hormonal options for managing menopausal symptoms also. Oestrogen [as part of hormone replacement therapy] is the most effective for treating symptoms such as hot flashes and night sweats and vaginal symptoms in addition to protecting against the development of bone density loss and osteoporosis.
“If the symptoms of menopause are not relieved by lifestyle changes, and they often are, we advise to talk to a doctor who has menopause training,” says Dr Lundy.
I’m menopausal and so anxious. Is this normal?
“It is extremely common to experience changes in your mood and anxiety with menopause,” says Dr Hartley. “Many women report a loss of confidence, low self-esteem, irritability or a loss of motivation. Sometimes these symptoms come and go and can be mild. For others, they can be debilitating.
“Women who have experienced depression, anxiety, significant premenstrual symptoms or postnatal depression/ anxiety in the past may be at higher risk of developing issues with mood or anxiety at the time of menopause. It is important to speak to your GP about the many options for managing all of these symptoms.”
Menopause is ruining my sex life. What can I do?
“This depends on so many factors,” says Dr Hartley. “What are the underlying issues affecting your sex life? Have you vaginal dryness that is making sex uncomfortable or painful? Are you suffering from poor sleep or low mood? There are many things that can impact on sexual desire and function. I would advise that you speak to your GP.”

I am full of rage! Why is this happening to me?
“There could be lots of reasons for this,” says Dr Hartley. “The fluctuating oestrogen levels that occur in perimenopause [the years of hormonal changes that lead up to menopause, the final period] may have a big impact on mood, irritability, anxiety levels and confidence. Oestrogen has an important role in our nervous system and has an impact on how we make neurotransmitters, the expression of hormone receptors in our brains and protecting our nerve cells from damage.
“Rage is not uncommon in menopause. It needs to be addressed with healthcare,” says Dr Lundy. “HRT may help, but sometimes menopause hormonal changes just spark the onset of underlying psychological disorders such as bipolar, severe anxiety and depression.
“Vulnerability to changes in mood or irritability are compounded by poor sleep, fatigue and other possible symptoms,” advises Dr Hartley. “Know that you are not alone and that there are lots of options available to help you manage.”
Is hormone replacement therapy right for me?
“This is a very difficult question to answer as it depends on so many different factors,” says Dr Hartley. “Menopausal hormone therapy [HRT] is one of several different management options we have for helping women alleviate symptoms of menopause. With HRT, there is also protection from bone density loss and, for some women, there may be a reduction in the risk of developing cardiovascular disease. It is dependent on your own background risk and what symptoms you are hoping to treat. It depends on your own health values and goals.
“For the majority of women, the benefits of hormone therapy, both for symptom relief and for health gain, outweigh the potential small increased risks. The type of HRT, what hormones are prescribed and how long you take them for is also important when looking at risk. Again, for most women, the benefits outweigh the risks. How long you take HRT for is also highly individual, and there is no arbitrary age or duration of use by which you have to stop your medication.
“It is important to look at lifestyle factors such as smoking, physical activity, alcohol consumption and diet, which can have an impact on the long-term risk of developing osteoporosis or bone density loss and cardiovascular disease.
“Having your blood pressure and cholesterol checked annually, keeping up to date with breast and cervical check screening is also vital. There are many alternatives to using HRT, but it will depend on what symptoms are impacting your quality of life and, therefore, the aim of treatment. Whatever route of treatment you choose, you should be well informed and have an in-depth discussion with your healthcare provider about what is the best option for you.”
How long until I feel like myself again?
“This is a hard question to answer,” responds Dr Hartley. “The duration and severity of symptoms is dependent on lots of factors and is highly individual. The average duration of hot flushes and night sweats is five to seven years. Most symptoms will improve with time, but some issues, for example, vaginal dryness and discomfort, may continue to get worse with time.”
Dr Lunday says: “Most women start to feel a lift by age 55-60. Others may be burdened much longer and, remember, some women may get no symptoms at all.”
















