What is it and who gets it?
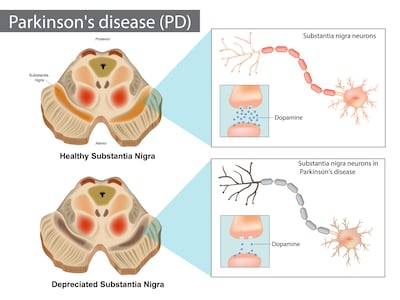
Parkinson’s disease is a progressive neurodegenerative disorder, caused by reduced levels of the brain neurotransmitter, dopamine. The second most common neurodegenerative condition after Alzheimer’s disease, Parkinson’s disease is also classified as a movement disorder as it primarily affects movement.
Although principally a disease in older age, about 30 per cent of those with the condition worldwide are under 60. The condition is slightly more prevalent in men than women.
What are the symptoms and how is it diagnosed?
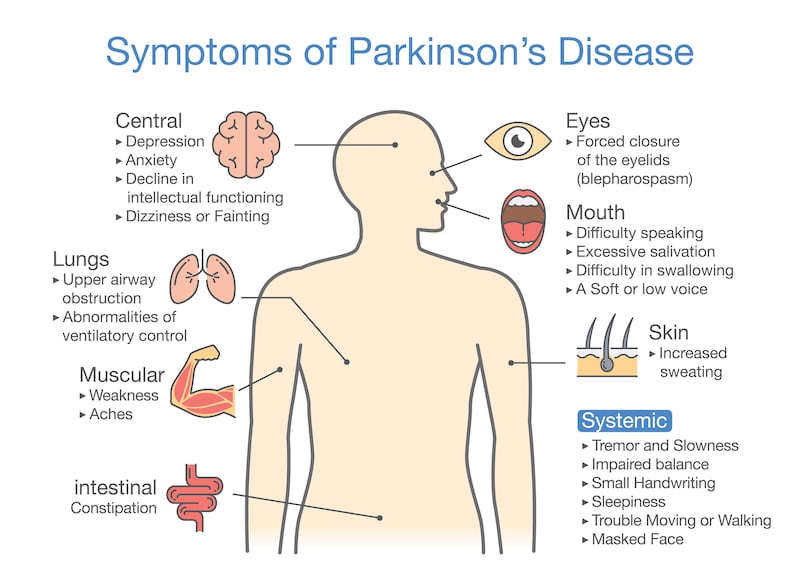
The main motor symptoms of Parkinson’s disease are tremors (the so-called resting tremor is often most noticeable in the hand), muscle stiffness and spasm and slow movements which sometimes result in short, shuffling steps when walking. Some sufferers also have poor fine-motor skills which impact on writing (small handwriting is common) and keyboard use, tying shoelaces and fastening buttons.
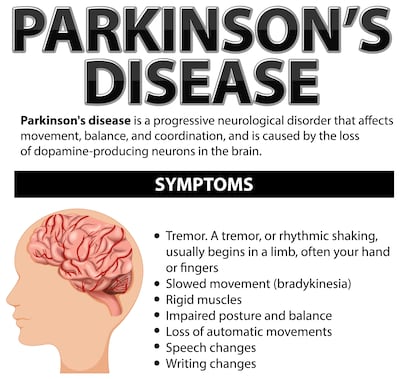
People with Parkinson’s can also suffer from a range of non-motor symptoms including anxiety/depression, constipation, bladder problems, low blood pressure, excessive sweating, fatigue, loss of sense of smell, memory problems, pain and sleep difficulties. Sometimes, these non-motor symptoms can appear years before or years after the motor symptoms and are not always identified and treated as part of the condition. The type, severity and combination of symptoms vary greatly from person to person and some of the non-motor symptoms can also be due to side-effects of medication. Many people with Parkinson’s develop dementia in the latter stages of the disease.
RM Block
The term Parkinsonism is an umbrella term that describes conditions with the main symptoms (tremor, muscle rigidity and slowness of movement) of Parkinson’s. About 85 per cent of people with Parkinsonism have Parkinson’s disease. The other 15 per cent have rarer conditions including Multiple System Atrophy and Drug-Induced Parkinson’s Progressive Supra-nuclear Palsy.
Prof David Bradley, consultant neurologist and clinical lead on Parkinson’s disease at St James’ Hospital, Dublin explains that diagnosis is based on clinical symptoms. “A patient with a hand tremor would [typically] be referred by their GP to a neurologist for diagnosis. It’s a progressive disease so symptoms arise over time but an early diagnosis helps us intervene earlier so patients can keep working and partaking in hobbies to maintain a good quality of life,” he explains. Parkinsonism is sometimes confirmed with a DaTscan. This involves a radioactive dye, ioflupane being injected into the blood which when it arrives in the brain can highlight abnormalities in dopamine production.
What treatments are available and how do they compare to treatments in the past?
There is currently no cure for Parkinson’s disease so different treatments focus on reducing motor and non-motor symptoms. Dopamine replacement drugs (levadopa and dopamine agonists) are prescribed in tablet or via a pump.
Deep brain stimulation is a surgical procedure available in Beaumont Hospital, Dublin, which improves the abnormal movement and tremors that many people with Parkinson’s disease have. The procedure – for which a pre-operative assessment is required – involves the placing of electrodes in the brain. These electrodes emit electrical impulses to brain circuits which regulate abnormal movements in the body.
Many people with Parkinson’s also need physiotherapy, speech and language therapy and occupational therapy to help them manage their daily activities.
Have there been any breakthroughs in treatment or self-management of the disease in recent years?
An app to help people with Parkinson’s monitor their symptoms and exercise and medications was launched in July 2023. Developed by dietician Richelle Flanagan, who was diagnosed with early-onset Parkinson’s in 2017, the My Moves Matter app aims to improve self-management and usher in more personalised care for people with Parkinson’s.
“When you live with Parkinson’s, everything matters – your diet, your exercise, your sleep and when you take your medications because they all make a difference to how well you can live day to day,” says Flanagan.
Flanagan is particularly keen to validate research that found women with early-onset Parkinson’s experience worsening symptoms in the week before and during their periods. “It seems that oestrogen receptors in the brain affect dopamine uptake,” says Flanagan who is currently seeking funding for research into how the peri-menopause and menopause impact women with Parkinson’s using data from the My Moves Matter app.
Currently, medication dosage doesn’t take into account such hormonal fluctuations. Flanagan is also keen to add dietary advice to the app because studies has found that taking medications too close to a protein-rich meal can reduce the update of levadopa.
What are the health services like for people with Parkinson’s disease?
While the number of neurologists has increased in recent years, it can still be difficult for patients to get appointments with neurologists quickly. Prof Bradley says that patients are generally seen in one of the five specialist centres in hospitals in Dublin, Cork, Galway, Limerick and Waterford within six months of their first symptoms.
A 2023 survey of access to health services among people with Parkinson’s found that one in five people took longer than 12 months to be diagnosed, with public patients diagnosed more slowly than private patients and those with early-onset Parkinson’s diagnosed more slowly than those with late-onset.
Once diagnosed, those with Parkinson’s disease see a neurologist once or twice a year so support between these appointments and self-management of the condition is crucial. The aforementioned survey found that, in the public system, one in five people with Parkinson’s had access to a Parkinson’s disease nurse specialist, six in 10 had access to a physiotherapist, four in 10 to occupational therapy and/or speech therapy and less than two in 10 have access to mental health supports and dieticians.
Voluntary groups such as Move4Parkinsons and the Parkinson’s Association of Ireland encourage people with Parkinson’s to join exercise classes, choirs and other social activities. The Women’s Parkinson’s Project also offers support to women with Parkinson’s through personal stories. The Movers & Shakers podcast (Spotify, Apple) is also a useful resource. There is also a support group in Ireland, Early Onset Parkinson’s Disease, (eopd.ie).
[ App aims to help women with Parkinson’s disease improve their quality of lifeOpens in new window ]
Richelle Flanagan, who volunteers with the Dublin branch of the Parkinson’s Association of Ireland, explains that many people retreat into their homes with the shock of diagnosis. “Parkinson’s wants to make your world small. It wants to make your voice small, your walk small, your writing small, everything small. So you have to do everything to make your world bigger by doing the things that motivate and stimulate you.”
What does the future hold for people with Parkinson’s disease?
It is estimated that about 10 per cent of all Parkinson’s disease cases have a genetic origin. “There are about 20 genes seen in young-onset Parkinson’s (ie those diagnosed in people in their 30s and 40s). There are multiple factors involved in the other 90 per cent of cases,” explains Prof Bradley.
There is much research into gene therapy and biological treatments which would slow down or stop the progression of Parkinson’s disease. However research into so-called disease-modifying drugs which prevent the initial reduction of dopamine production in the brain is not at an advanced stage.
[ Parkinson’s disease: Health system gaps must be filled to treat varying needsOpens in new window ]
Other studies are investigating possible biomarkers which, if found in the blood, urine, cerebrospinal fluid, saliva or gut or via an imaging, voice or light-sensitivity test, could identify those susceptive to Parkinson’s before they develop symptoms.
“People have lost about 70 per cent of their dopamine neurons by the time they develop a tremor so when we have really effective treatments (eg drugs to slow down or reverse nerve damage) to prevent the condition developing, it would be beneficial to have a test to screen people in mid-life before the condition gets established,” says Prof Bradley.



















