The first sign of trouble for Ciaran Davis was mouth ulcers. Even if he had not been a self-described “clueless” teenager at the time, he could never have guessed they were to herald a lifelong bowel disease.
But when medical pastilles did not clear the ulcers and then he was floored by fatigue, his GP referred him to an endocrinologist (in hindsight it should have been a gastroenterologist).
The next step was tests as a hospital inpatient.
“I started the whole series of really mortifying, really embarrassing experiences of doctors doing things, putting tubes down you, up you, fingers down you, up you, and things like that,” he recalls.
RM Block
They also did a laparotomy (surgical incision through the abdominal wall) to take biopsies, but still struggled to identify the problem.
“It took me about six or seven months from the onset of symptoms to be diagnosed definitively with Crohn’s, which isn’t bad,” says Davis.
Although, in the meantime, he had become anaemic and lost a lot of weight.
Not only had he never heard of the disease, nor had his mother, who was a nurse. But that was more than 30 years ago, when the gut was not mentioned in polite conversation. Now, if he refers to Crohn’s disease, invariably another person will know somebody else who has it.
However, inflammatory bowel disease is still not widely spoken about because you are talking about poo, says nurse specialist Angela Mullen candidly. But she welcomes how social media and an upsurge of interest in gut health and the microbiome have helped to open up the conversation.
At least 40,000 people in Ireland are living with inflammatory bowel disease (IBD).
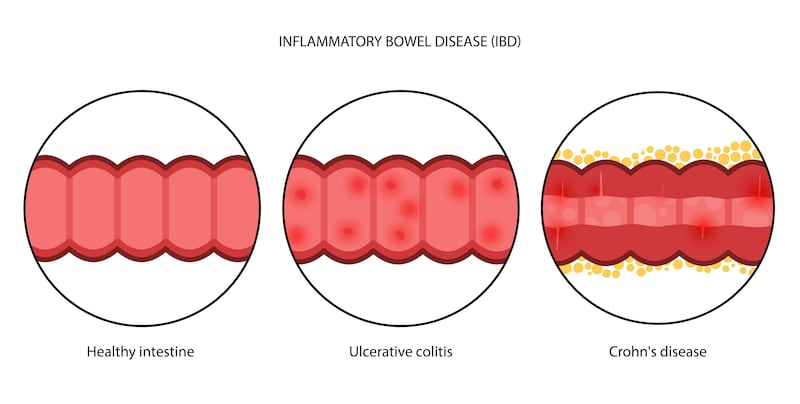
The two main types are:
- Crohn’s disease, which occurs in patches in any part of the gastrointestinal tract running from the mouth to the anus
- and ulcerative colitis, which affects the colon (large intestine).
The cause is unknown but there is believed to be a genetic predisposition, which is triggered by environmental factors. Despite a similarity in acronyms, IBD is not to be confused with irritable bowel syndrome (IBS).
“Some of the symptoms overlap a lot, like pain, bloating and altered bowel habits,” says Mullen. But with IBS, many of those signs can be food related and there is no inflammation. The differential is bloody diarrhoea, mucus and urgency, she says. Inflammation, particularly in colitis, is likely to cause bleeding.
For those with suspected IBD, there is a test that measures protein levels in the stool.
“If that is elevated, you have got inflammation,” Mullen explains. “Then we go searching for it.” The “gold standard” tests of colonoscopy and biopsy will be done. “These combined together will give us a definitive diagnosis.”
From the onset of symptoms, it is likely to take up to a year for diagnosis because, initially, Mullen suggests, people tend to think they just have a bug when first hit with bouts of diarrhoea. Few people would go rushing to their GP. But if there is bloody diarrhoea, she reckons cancer is going to be everybody’s first thought.
“Depending on who you are and what’s your mindset, you either ignore it or you act.” Of course it should be the latter.

Working in Cork University Hospital (CUH), Mullen is one of about 30 members of the Inflammatory Bowel Disease Nurses Association of Ireland, which was set up 10 years ago. She is part of a multidisciplinary team at CUH treating patients who come to them through the hospital’s acute services or via clinics. Generally they see them twice a year but “if you are more acute we will see you more often”.
A big part of her job of as a nurse specialist is keeping patients with IBD out of hospital. They are considered in remission when they are well but just daily living can cause a flare-up, she explains. Stressful times, such as doing exams or getting married, may be triggers; also common medications, such as certain painkillers and antibiotics.
“Then they would contact someone like me and we would try and manage it as much as we could, without having to even come into the hospital. A lot of it is virtual management. I’ve known patients who have been nervous to leave their house,” she says, empathising about how difficult it must be to travel when “all you’re concerned about is where is the nearest toilet”.
Concerts and festivals would be a nightmare.
“To be truthful, actually, it’s a life-changing, life-limiting condition,” continues Mullen. “Our objective in all of this is for people to live their best lives in whatever way, shape, or form that is. For them to get on and go and travel the world if they want to. Or go to college, play their sports.”
Over years working in this area, she has seen the development of a wide array of very effective medications to treat IBD. Access to services can still be problematic for patients and it is not one of the long-term illnesses recognised for an automatic medical card. That can be financially tough for people, she points out.
“Once you’re in the public [health] system, it’s a great system. I know people give out about it all the time but once you’re in it, it’s amazing. It’s getting into it is the challenge.”
Mullen also believes it’s important that we talk about IBD, even if is regarded as a topic few want to hear about or discuss. Raising awareness is important not only for informing those living with the condition, or experiencing symptoms, but also for wider societal understanding and empathy.
Crohn’s and Colitis Ireland (CCI) has been working on that for the past 40 years. On August 12th a special final episode in the fourth season of Gutcast, a podcast created by CCI and Johnson & Johnson, is being released to mark the 40th anniversary celebrations (episodes available on Apple, Spotify and janssenwithme.ie). Hosted by Amy Kelly, who has Crohn’s disease, the podcast portrays a much more positive picture of living with IBD than the scant, seemingly gloomy information Davis was given when he was diagnosed.
“I was scared for the future at the time, I didn’t really know what to expect,” he says.
Davis believes it is important to be able to hear people’s stories. The more upbeat approach taken by CCI, of which he is a board member, is “not trying to deny reality”, he stresses.
“It can be very difficult at times but if you follow the right instructions, you can get back to normal, and there is light at the end of the tunnel. You’ve got people who are living with Crohn’s and with colitis who are running marathons and climbing mountains.”
As well as running a helpline (01 531 2983) three mornings a week and promoting peer support, CCI issues a “No Waiting” card, which discretely requests urgent access to a public toilet for the holder. The organisations calls on businesses and public amenities to support people with IBD by recognising this card and facilitating access for individuals.
Being diagnosed during early adulthood was hard psychologically for Davis, as his peers were all out enjoying themselves. While patients can be diagnosed at any age, from babies upwards, incidence peaks between the ages of 15 and 35, with another smaller peak in the 50 to 70 age range.
Davis had wanted to return to studying for a degree at night, having taken up a bank job after his first year in university. But he was exhausted and, although his employer was very good to him over sick leave, he despaired of ever being able to further his education.
“I was extremely sick and, at 6ft tall, down to 8st in weight, having lost 3st.”
He was having very bad night-time fevers, which seems to be one of the less common symptoms of the condition.
Living in north Dublin city, Davis has been in what his doctor terms “deep remission” for the past eight years. Before that, he typically experienced flares every five years, which generally came on very quickly, but also responded relatively speedily to treatment. However, he has had to have surgery to remove a section of small intestine that had become hard and scarred by inflammation and is on long-term medication.
Many people feel it impacts their social life, family life, intimate relations, educational aspirations, career aspirations – but it doesn’t actually have to be that way
— Ciaran Davis
He finds following a varied but fairly bland, low-fat diet as much as possible keeps him well. In earlier years, he believes stress could have been a trigger for flares but as he gets older he feels more resilient. Davis, who has recently started an IT job with the Sustainable Energy Authority, also believes it is important to work with good people and find a workplace compatible with managing what he describes as a “transient disability”, in that he is prevented from doing things when unwell.
Through his volunteering with CCI, he had the opportunity to go to the United States to train in the Stanford chronic disease self-management programme.
“Many people feel it impacts their social life, it impacts their family life, intimate relations, educational aspirations, career aspirations – but it doesn’t actually have to be that way. There are ways in which people can mitigate the symptoms, or the impact of the symptoms, and also gain the confidence – or self-efficacy is what we call it – to self-manage around their own symptoms.”
Now a master trainer with HSE’s Living Well – a six-week group, self-management course for adults with long-term health conditions – Davis is clearly glad to be able to use his years of living with IBD for the benefit of others as well as himself.
“The more experienced you are at your job, the better you are,” he adds, “and the more experienced you are living with a health condition, the better you are as well.”
Common symptoms of IBD
- diarrhoea
- stomach aches and cramps
- blood in your poo
- fatigue
- weight loss
- anaemia
- nausea/vomiting
- mouth ulcers



















