Ireland’s spending on health is towards the top of the international league, as a percentage of national output. But the latest Covid-19 wave has underlined the ongoing shortage of hospital capacity, particularly for intensive care unit (ICU) beds. So why has the big ramp up in health spending in recent years not delivered in terms of some of the key services – not only ICU beds but also accident and emergency (A&E) capacity and waiting lists for some key procedures? Before the crisis hit, ICU bed capacity here was near the bottom of the Organisation for Economic Co-operation and Development (OECD) league.
A new report from the Irish Fiscal Advisory Council (IFAC) sheds some light, and raises some questions, which are vital to ensure the planned increases in spending in the years ahead pay-off in terms of better services.
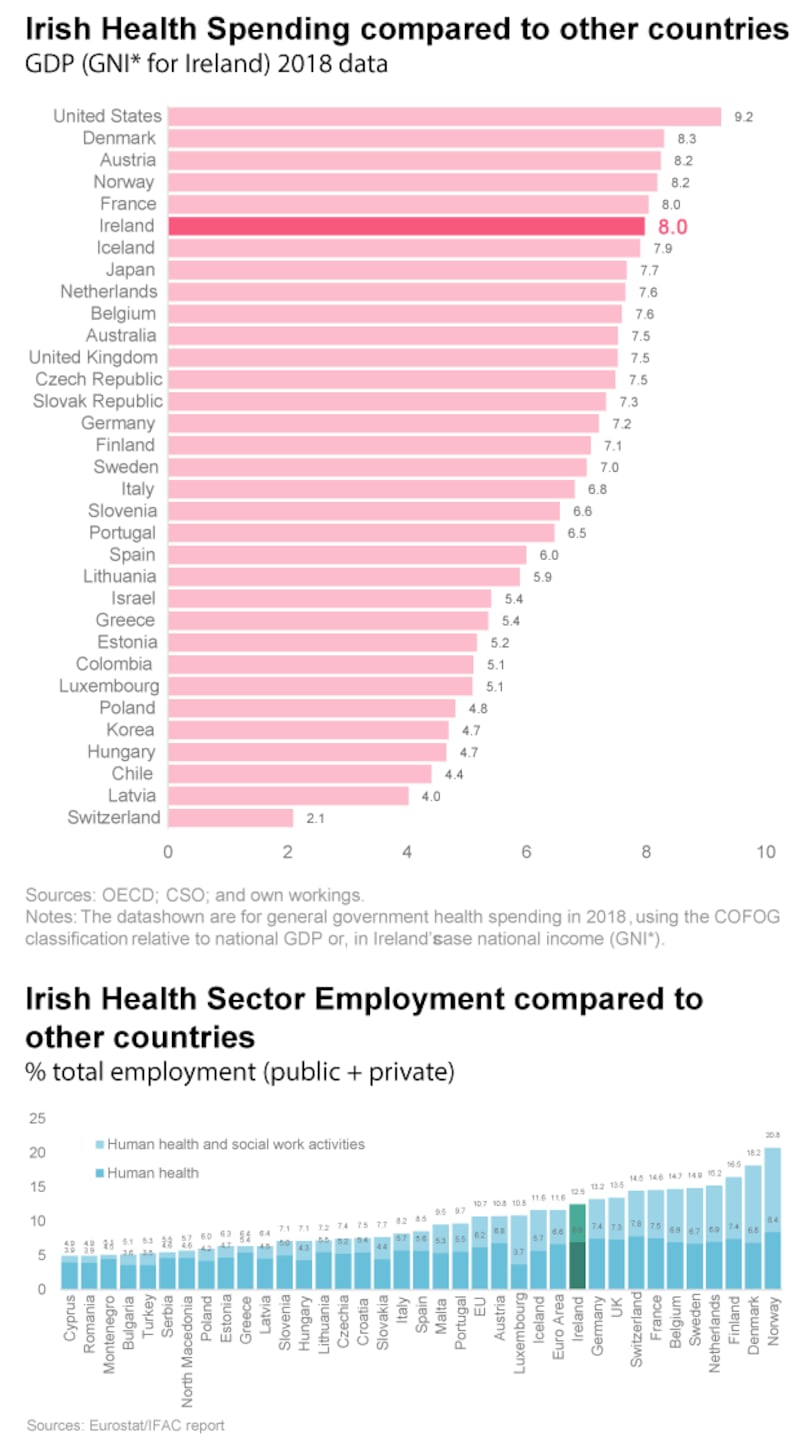
The IFAC report, by Dr Eddie Casey and Killian Carroll, points out that Irish health spending has risen over many years, increasing from about 2 per cent of national income in the mid-20th century to around 8 per cent now. Ireland ranks sixth for government spending on healthcare as a share of national income out of 33 OECD countries (there are some caveats here, as we will discuss below). Health spending has increased relatively quickly here compared to other countries in recent years, even though Ireland has a younger population than many other countries. It now accounts for 30 per cent of total spending, compared to 10 per cent in the early 1970s – and a sustained rise in life expectancy has continued over the same period. Over the last 25 years alone, health spending per capita, adjusted for inflation, has increased by over 800 per cent.
So why is health spending rising so rapidly?
1) Longer-term factors behind health spending rise
An ageing population and rising incomes are generally seen as the two key factors pushing health spending higher. The IFAC researchers believe these have had a role here, but do not explain a significant part of the increase. Other key factors are likely to be improved drugs and treatments and policy reforms like Sláintecare. The researchers also point out that healthcare must compete on the open market to attract staff, but that by its nature productivity improvements in the sector can be relatively slow. And so healthcare becomes costlier to deliver. But they argue that it is hard to get behind the full reasons why health spending has risen so quickly. Ireland spends relatively highly on outpatient services and health capital investment overall is around the average. But despite this, there has been a lack of ICU beds for many years with Ireland having five beds per 100,000 in 2019 – France had 16 and Germany 27. Irish ICU bed numbers have ramped up from just over 200 in 2019 to around 300 now – but pressure will remain to continue to increase this. Health service employment here is also in line with international norms.
2) The impact of high cost Ireland
A 2021 ESRI paper by Maev-Ann Wren and Aoife Fitzpatrick looks at some different measures by comparing health spending. It looked at total healthcare spending by both the private and public sector, and so differs from IFAC which focused on Government spending. It shows that in 2017 health spending in Ireland as a percentage of national output was the highest in the EU. But looking at per capita spending and adjusting it for the different price levels in different countries dropped Ireland down to ninth. This gives an indication, they say, of the actual amount of health services from which people benefit – and the impact of higher prices and costs in Ireland.
The researchers wrote: “Our analysis leads us to conclude that the dichotomy between Ireland’s apparently relatively low volume measure of per capita healthcare consumed and relatively high measure of the proportion of national income expended on healthcare reflects relatively high prices and wages in Ireland.”
We know, as the ESRI paper points out, that the cost of living in Ireland is one of the highest in the EU. And that other costs – such as in areas of construction – are relatively high here also. In general, this means money spent does not go as far in Ireland. However, the most obvious issue relates to pay – whatever the debate about precise rates of pay, it is clear that a higher pay level is needed here if healthcare staff are to have the same standard of living as those in other countries. And high rental and housing costs are a particular issue and also make it more difficult to attract staff to Ireland from overseas. Part of the issue in expanding ICU bed numbers during the pandemic has been attracting enough staff.
3) The problem of planning
Ideally, higher spending is planned and delivers improvements in service levels. And clearly we have just seen the greatest exception in terms of planning – the pandemic could not have been foreseen and required a big and rapid increase in spending.
Some of this extra spending is one-off – but a higher level of health spending will now persist, partly because Covid-19 is not going anywhere soon. But the pattern of spending overruns before the pandemic, examined by IFAC, showed a lack of planning and control in normal times. Between 2016 and 2019 health spending continued to overrun by an average of €590 million a year, meaning that much of the increase was unplanned. Typically, inadequate amounts were allowed each year, especially for hospital budgets, where average annual increases of 0.8 per cent were, according to IFAC, “far below the likely cost of maintaining the existing level of service”. By the end of the year, the budgets had been bust, with the bulk of the overrun on pay costs. Much of this extra money was needed to maintain service levels, but haphazard controls are not likely to lead to ideal results, or improvements in service levels. The bills were paid by a constant overperformance of corporation tax revenue.
4) The future and Sláintecare
The big jump in activity levels during the pandemic has seen activity levels in hospitals rise and put the system and staff under pressure. Their resilience in dealing with what has happened has been remarkable. Debate on where the gaps have been and what needs to happen will come next, with a rise in the number of ICU beds planned, albeit from low levels by international standards.
But there is also the major Sláintecare plan, the reform plan for the health service agreed by all the main parties. Recently Taoiseach Micheál Martin has said on a number of occasions that he is committed to the “principles” of the plan. But what does this mean?
Remarkably, the IFAC research finds that “basic information is severely lacking” on the plan, no updated costings have been produced since 2017 and little clarity on progress made is publicly available. The reforms were estimated in 2017 to add some €2.8 billion to the annual cost of providing healthcare. IFAC speculates this figure may now be higher. But we don’t know. Meanwhile an ageing population will slowly be steadily push up healthcare costs anyway.
The researchers welcome recent Government plans to limit spending increases to 5 per cent per annum up to 2025 and to budget more realistically for maintaining existing service levels. But they say proper long-term budgeting in health is now essential and that, unusually, this year’s budget did not set down a spending ceiling by the department for the next three years.
The response of the health system to the Covid emergency has been remarkable. Now the challenge of building a better system for the future needs to be faced.














